It all started as a little cough. It wasn’t too bad so I didn’t think too much of it and procrastinated seeing the doctor about it. More than 2 months later, the small “tickle of the throat” cough turned into a stronger, spastic cough. I was 14 weeks pregnant at this point and the cough was now disruptive to my everyday comfort. I also noticed I started having some shortness of breath, fatigue, and itchy skin but figured it was due to the pregnancy. I did find the shortness of breath unusual since I was still regularly working out and teaching fitness classes.
Disclaimer: if you don’t want a TL;DR version, you can stop here and know it all started with a cough. If you want the full version, keep reading!
Over the course of the next 6 weeks, doctors tried to treat my cough as asthma, allergies and a sinus infection, with the limitations of medications available to a pregnant person. Nothing improved. Every doctor I visited listened to my lungs through their stethoscope and said my lungs sounded clear. I had been through inhalers, tons of different allergy medications, and three rounds of antibiotics. My cough continues to be powerful, riveting my whole body to the point where I fractured a rib. I tried to be patient with each of the different treatments we tried, eagerly hoping one of them was “the one” to solve my cough. I also started getting winded just walking up a flight of stairs. This was unusual for someone who regularly worked out, I thought.
Nothing worked. My symptoms got worse and my body was in pain from constantly coughing.
When Benefits Outweigh the Risks
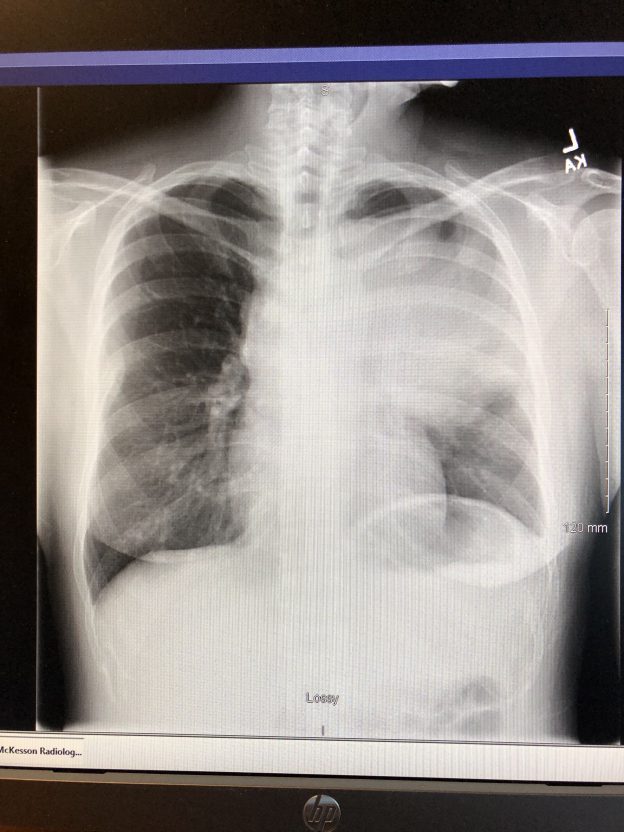
Finally, one of my doctors said we were at the point that we needed a chest X-ray if we wanted to find out more. I hesitated. X-ray? Pregnant women aren’t supposed to get X-rays, I thought. It’s just not safe! I consulted with my obstetrician and he said at 20 weeks pregnant, it was okay as long as they shielded my abdominal region. I moved forward with getting my X-ray.
Within an hour, I got a call from my doctor with results. He said there was some sort of large mass around my left chest. It could possibly be pneumonia or a tumor, but he couldn’t confirm from the X-ray, but there was definitely something abnormal. Both of these possible results sounded awful. He told me to come in the next morning ASAP to further discuss with my regular PCP (the doctor that got the results was my PCP’s backup since she was out that day). I remember hoping it would be pneumonia because I thought that would be much more treatable than a tumor.
My doctor explained that she needed a CT scan to be able to tell what the large mass in the X-ray is. CT scans have incrementally more radiation than an X-ray. Is this safe for the baby? As a mom, we constantly have the mental battle between sacrificing ourselves for the sake of our child. My doctor consulted with my obstetrician and he said that a CT scan would be okay as long as they took extra precautions such as shielding my abdominal region and minimizing contrast used. He also explained to me that based on my X-ray results, we were at a point where we needed to weigh the risk vs. benefit of what I potentially had. In order for the baby to be healthy, I needed to be healthy.
The C Word
My CT scan was scheduled the following morning. Within two hours of doing my CT scan, my doctor had the results and called me. I remember being at work and having to find a quiet place to sit down to talk to her. She explained it was a 14cm mass sitting on top of my left lung, pressing against some of my vital airways and blood vessels. This was why I was coughing and having shortness of breath. She wanted me to meet an oncologist with MD Anderson ASAP because a biopsy of the mass was needed to determine if it was cancerous. Cancer. That word alone is scary.
Thanks to my doctor’s quick action and sense of urgency, I was able to see an oncologist at MD Anderson in the next three hours. Due to my pregnancy, my situation was prioritized.
My world was spinning at this point. In less than 48 hours, I went from thinking I had a sinus infection to possibly having cancer. We met with the general oncologist at the MD Anderson Sugar Land location. She explained that the “ideal” situation would be that the mass could be lymphoma, which is very treatable with chemotherapy, even during pregnancy. If the mass was actually benign, surgery would actually be more complicated to remove it due to its close proximity to my heart and other major blood vessels.
I wasn’t sure what to think of those possibilities presented to me. Both sounded awful. The next necessary steps were for me to get a biopsy of the mass to confirm if it was cancerous. The oncologist and radiologist had to evaluate how to do this biopsy. There are noninvasive, efficient ways to do a biopsy, but they involve radiation. These weren’t an option for me due to my pregnancy. The radiologist said he could instead do a biopsy using an ultrasound and find a place to extract the mass tissue. This is usually done under general anesthesia, but because of my pregnancy I opted to do it under local anesthesia to reduce more drug exposure to the baby. I remember feeling extremely nervous about the biopsy. Was it going to hurt? Could I tolerate the pain?
The biopsy was done a few days later, the week of Thanksgiving. They used lidocaine to numb my chest area and got to work on the biopsy. It was painful, even with the lidocaine. Due to the mass, I have a hard time laying flat without coughing compulsively. This, coupled with the biopsy pain and discomfort, was hard. It was finally over and I felt a sense of relief. One obstacle down, but there were many more to come.
And We Wait
I tried to enjoy Thanksgiving as much as I could. It was hard to lie to well-meaning relatives asking me if I was okay and why I was still coughing so much. I told them it was allergies to try not to worry them.
While I waited for the biopsy results, there was a lot of praying and reflection. Deep down, my intuition told me that I thought I had cancer. Roberto and I prayed it could be something else that was treatable. But for some reason I had the lingering thought that it was cancer.
An Answer and a Plan
A week after the biopsy, at 22 weeks pregnant, I got a call from my oncologist on the results. She confirmed it was lymphoma. Specifically, I had a non-Hodgkin Lymphoma called primary mediastinal large B-cell lymphoma. She explained to me that getting chemotherapy treatment pretty soon was necessary due to the size of the mass. She didn’t know the stage of the cancer, as this requires additional tests like a PET scan and bone marrow biopsy. Due to my high risk situation with my pregnancy, she wanted me to be seen soon by a lymphoma specialist at the MD Anderson main campus for a consultation.
I was at work and in shock. I didn’t know what to do. I called my mom and told her the sad news. My mom was devastated. She told me she wished it was her instead of me having to go through this. I remember my dad calling me shortly after to tell me that my mom had told him the news. He told me he had no words, except that he was here for me. I held back my tears. Roberto and I left work early to absorb the news privately.
I am eternally grateful for all of my medical team who treated my situation with such urgency. It is thanks to them that I received immediate, customized medical care. There are many people who cannot even get admitted to be seen at MD Anderson, the #1 cancer treatment center in the country, and I had an appointment within hours. I was able to see the lymphoma specialist the next day. This day happened to be our fourth wedding anniversary.
My obstetrician called me and said he learned the news from my general oncologist. He recommended I look into maternal fetal medicine specialist who was experienced with high risk pregnancies. But because my case was so rare, he didn’t know any that were experienced with cancer patients.
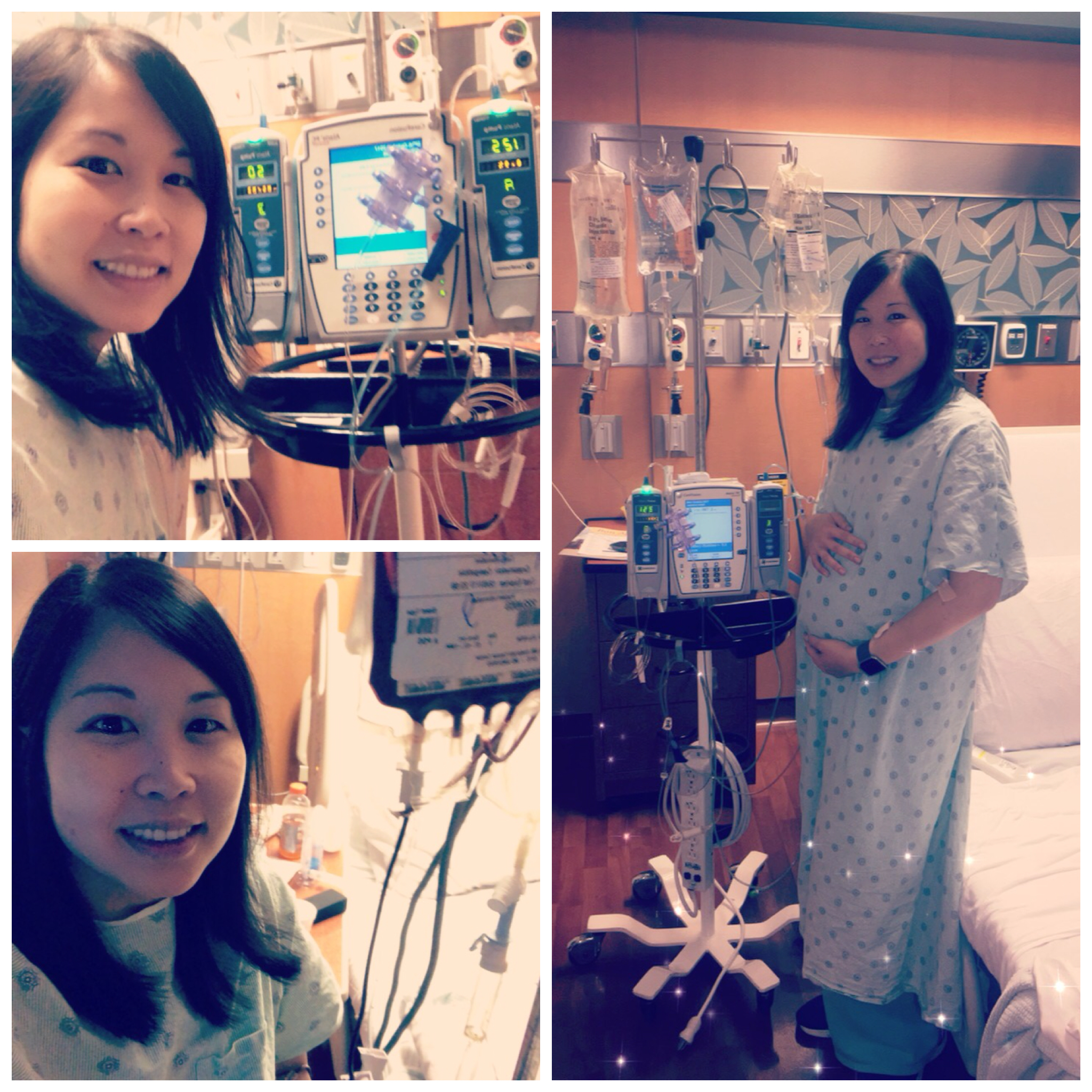
We met with the lymphoma oncologist who I later learned treated the most pregnant lymphoma patients in the practice. I felt I was in the right hands. She immediately got down to business and explained to us what chemotherapy treatment I needed and that I needed to start it the following week. I was blown away. In 5 days, I needed to start chemotherapy?! She explained the mass was so large and pressing against major airways and blood vessels that we couldn’t afford to wait.
The chemotherapy treatment recommended for me is R-CHOP, which is safer for pregnancy than other chemo treatments that are used for my same diagnosis. I would have six chemo treatments, once every 3 weeks. This amounted to about 18 weeks of chemo, which ironically was the same amount of weeks left in my pregnancy.
The lymphoma oncologist also recommended a maternal fetal medicine specialist that was experienced with cancer patients. They would work together to ensure each chemo treatment is going well for me and baby. After later meeting with the maternal fetal medicine specialist, she explained that our goal was to have four chemo treatments, wait three weeks, deliver at about 35-36 weeks pregnant, and then finish my last two chemo treatments.
Being the planner I am, I felt relieved we had a plan now to start my treatment. Seeing the chemo and pregnancy plan in small increments made it feel achievable and less intimidating.
What’s Ahead
So that’s my story of how it all started. The road ahead is scary and full of unknowns. But what I do know is I choose to be strong because being anything else at this time is not a choice for me and my baby.