Before my cancer diagnosis, Roberto and I went through another scare related to this pregnancy. We had a non-invasive pregnancy test (NIPT) that came back with a positive result for Down syndrome. We have now learned that this result was actually related to my cancer diagnosis. I am sharing this experience in hopes that it helps other families affected, as there is minimal information out there linking cancer and NIPT results.
Disclaimer: no personal beliefs regarding Down syndrome or pregnancy termination are expressed in this post.
Yay! We’re Pregnant!
I was very fortunate to have a healthy pregnancy with Camila. I taught group exercise classes, lifted weights, and did Zumba until I was 38 weeks pregnant! I had no pregnancy issues. I figured since I was still in pretty good health and fitness and delivered a healthy baby, my second pregnancy should be smooth too. I was hoping to be active through my pregnancy to have a strong body ready for labor and delivery. Surely these things would lead to a healthy baby.
I went ahead and scheduled my prenatal care for the first trimester. We had two ultrasounds done and both looked good. We elected to do optional first trimester genetic screening testing, known as Non-Invasive Prenatal Test (NIPT). For those unfamiliar with this test, it screens if there is missing or extra chromosomes 13, 18, 21, or sex chromosome. It is a screening test, meaning it gives you a risk of having one of the above conditions; it is not a diagnostic test. Well known companies that offer this test include Natera, Progenity, Harmony, and MaternT21. It is also a way to find out the gender of the baby early on in pregnancy. Roberto and I agreed it was important to do the NIPT test before we made our pregnancy announcement to be sure we had a healthy baby on the way.
Third Time’s a Charm
At 12 weeks pregnant, it was time to do the bloodwork for the NIPT. Because my insurance provider had changed since my first pregnancy, I was directed to use Natera’s Panorama test as that was the in-network NIPT for my insurance provider.
The day prior to having my NIPT test, I got a bad bout of food poisoning. I didn’t want to delay the NIPT test any longer, so I ate some crackers and drank some gatorade, headed to the lab, and got my blood drawn.
It took 10 days to get our results. The nurse called me and said the Natera Panorama test came back and it said “No Results”. What could this mean? It said there was some sort of laboratory error and they needed me to provide another blood sample. UGH! I figured it was because I had food poisoning. I felt like I wasted 2 weeks and we wanted to make our pregnancy announcement soon since I was starting to show. During this time, I also found out my insurance would not be covering the NIPT costs since I was not considered a high-risk pregnancy, so the cost would be out of pocket.
At 14 weeks pregnant, I went back to the lab and did a redraw to have my blood sample sent in again. We waited another 10 days for the results. One morning, as Roberto and I were driving to work, I checked the Natera portal and saw the results were ready. We had been wavering back and forth if we would do a gender reveal party when his family comes to visit. If I open the results, I would see the gender of the baby. I was so eager that I told Roberto I didn’t want to wait and begged him to let me go ahead and open the results instead of waiting for the doctor to call. He obliged and we opened the results together.
The results said… NO RESULTS. Again. How could this be? Two inconclusive test results in a row. This time, the results said that there was a DNA pattern that could not be interpreted. What does this mean? Does this mean there is actually an issue with the baby or is it a lab error? I had also started to get sick recently with a bad cough (hint: the start of my cancer symptoms). Maybe it couldn’t read my DNA because I was sick and on various medications?
We had a checkup with our OB the following day. He said it was very unusual to get no result twice. However, he assured me for my age, I had less than a 1% chance of having a baby with a genetic disorder. He said it was up to us if we wanted to try another NIPT test. We still wanted to, even if it meant paying more out of pocket. We opted to go with Progenity, the same test I used with Camila.
So now at 16 weeks pregnant, I got my third NIPT test. We were hoping this would be the final one. I was also very much showing at this point and several people at work were suspicious. I told Roberto I wanted to go ahead and start sharing with people that I was pregnant because I really couldn’t hide it much longer. We both originally wanted to keep our pregnancy news private until we received the NIPT results, but since it was taking so long, I felt like I needed to go ahead and tell people. Roberto discouraged me from doing it, but I went ahead and shared the news with more friends and my coworkers. Prior to this, only close family and friends knew.
The Results
In just 5 days, my obstetrician called me on a Friday I was off work. He said my Progenity test results came back with a high risk of the baby having Down syndrome (extra copy of chromosome 21). The world completely stopped moving. How could this be? I’m healthy and only 33 years old; I have less than a 1% chance of having a baby with a genetic disorder. How could this happen? I asked my doctor how accurate this test is. He said they are usually pretty accurate, though it is a screening test to assess risk and not a diagnostic test to confirm a result. Is it possible the test is a false positive? Very unlikely, he said. My OB explained my options on what I could do next if I wanted to do additional diagnostic testing to confirm the NIPT test.
I tried to process it, but a million different thoughts raced through my mind. Was I fit to be a mother to a special needs child? Would it be hard on Camila to live a life with a sibling with Down syndrome? I already feel like I’m struggling now with a healthy child. How can I do it with a child that needs more? Other thoughts crossed my mind. Should we have a special needs baby knowing that we are not prepared? Could I live with myself if I terminated this pregnancy? What would I tell everyone when they ask what happened? They all know I’m pregnant now.
I called Roberto at work to tell him the news. I could not keep myself together. He came home from work and we cried together. We only wanted a healthy baby and now nothing was guaranteed for our family. We looked at the Progenity test results together and that’s when we learned the baby’s gender in the least exciting or joyous way. It’s a boy. It was hard to be excited knowing the challenges our family would face.
We shared the news with my parents. It was extremely difficult to look at my parents and tell them that there could be something wrong with the baby. My mom told me exactly what we needed to hear–that she would support us no matter what we chose to do. Our joy was their joy, and our sadness is their sadness. My dad prayed to his mother that everything would actually be fine and he said that his mom has never let him down we he needed her. Roberto also shared the news with his parents, but very lightly as he did not want to worry them. They said they would pray for us.
At this point, praying was all we could do. The reality is if the baby has Down syndrome, that already developed long ago in the beginning of pregnancy. There was nothing we could do to reverse it. For those not familiar with Down syndrome, it occurs randomly. It’s neither the mother’s nor the father’s fault and there is nothing you can do environmentally or behaviorally do to prevent it.
We had several plans that weekend and had to put on our best poker faces. We got asked by well-meaning friends if we were excited for baby #2. I had to avoid taking pictures because I didn’t even know if I was going to be pregnant much longer. We felt so helpless because there was nothing we could do but wait until the week to start to see specialists for our situation. We both did our fair share of Googling to read all sorts of stories that made our imaginations run wild. And there were lots of tears over the weekend. The one thing that kept us together was our shining light, Camila. She is so happy and full of life. We are so blessed to have her. Maybe she’d be our only child, because I don’t know if I could go through this again.
More Testing
The following Monday morning, I get to work and start calling the maternal fetal medicine specialists that my OB’s office referred me to. I am desperate to get an appointment as soon as possible. I am 17 weeks pregnant at this point and I feel like time is running out for us to make a decision on what to do next if we were to consider other options (we never said what we going to decide on what to do until we were faced with a confirmed diagnosis). I am able to get an appointment the following day at the High Risk Pregnancy Center at Memorial Hermann Sugar Land. They explained to me that they would do a level 2 ultrasound, we would talk to the a genetic counselor, and if I decided to proceed, I could even do an amniocentesis that day. An amniocentesis is an invasive prenatal diagnostic test that uses amniotic fluid to test for chromosomal abnormalities. It is a highly accurate way to confirm if the baby does have Down syndrome or other genetic disorders.
We get to our appointment at the High Risk Pregnancy Center. There are so many emotions running through us. We’re scared, hopeful, nervous, sad, confused. The first thing we do is the level 2 ultrasound. This is similar to the anatomy ultrasound normally done at 20 weeks. We look at the entire baby and the ultrasound technician takes measurements and close-ups to identify any soft markers for Down syndrome. The high risk pregnancy OB reviews our ultrasound and confidently says the baby looks healthy! There are no soft markers showing up for Down syndrome! However, we can’t fully celebrate yet. About 50% of babies that do have Down syndrome don’t show any soft markers in their ultrasound. We are at least going in the right direction of good news though.
Next, we speak with the genetic counselor. She starts from the basics of genetics and we go over all three of my NIPT results. She explains that an NIPT test only tests for a limited set of genetic issues–specifically trisomy 13, 18, 21 (Down syndrome), and sex chromosomes. We have 23 sets of chromosomes, so it does not test for the others. NIPT test also reads placenta DNA, which is not necessarily the same as the baby’s actual DNA. She explains to us that since the second NIPT test I took had a result of DNA not being able to be read, it presents another situation to us. It is possible that my second NIPT test could not be read because perhaps there is an issue with a chromosome outside of what an NIPT test would pick up. So now, not only are we worried about the possibility of the baby having Down syndrome, but the baby could actually have another genetic issue due to another chromosome having an issue.
Both Roberto and I are in agreement that we do want to have more diagnostic testing done in order to confirm the baby’s state. The genetic counselor suggests in order to do this, we do an amniocentesis and then order three tests:
- The FISH test is a rapid result test that can accurately diagnose if the baby does or does not have trisomy 13, 18, 21, and any sex chromosome issues. It will basically confirm the NIPT results. The turnaround time on this test is 1-2 days, which would be a great way for us to get some quick preliminary results.
- A chromosome microarray (CMA) can look for extra (duplicated) or missing (deleted) chromosomal segments for all chromosomes as well as mosaicism in the chromosomes. This test can confirm if there are any issues with all chromosomes as it relates extra or missing segments. It takes 7-10 days for this test result to come in.
- A karyotype will review of all the chromosomes to make sure we only have a pair of all 23 chromosomes (no extra or missing chromosomes). This test takes the longest to be completed at 10-14 days. These three tests would give us high assurance and accuracy if there are any genetic issues with the baby.
The genetic counselor noted that nothing is guaranteed when it comes to testing a fetus. There could be other health issues that these genetic tests do not cover. The only way we would ever know if we truly have a healthy baby is on delivery day.
We asked the genetic counselor what was the chance the NIPT is a false positive. We thought this was the only way we could ever get the positive outcome we longed for. She said it can happen, but it’s not common. When it comes down to it, I think it’s a 1% chance of there being a false positive. The odds aren’t in our favor.
The genetic counselor never pressured us to go with one option or another. She laid out all of our options and let us decide what was right for us. We decided to immediately move forward with the amniocentesis and the three tests she recommended. They outlined the risks associated with having an amniocentesis which included a very small chance of miscarriage. In fact, several moms decline having an amniocentesis because they don’t want to risk miscarriage. We accepted the risks and moved forward.
The amniocentesis procedure itself took less than 15 minutes in entirety. They did another ultrasound to identify the baby’s position and then stuck a long needle into my abdomen to pull a small sample of amniotic fluid. It hurt but was over quickly. We went home feeling sad thinking about how in a couple of weeks we may be faced with a difficult situation ahead for our future as a family. We were also hopeful that there was a small chance of a miracle happening with a false positive.
Waiting for Results
My cousin Julie’s wedding was that weekend and we agonized about how tons of family and friends would be asking about my pregnancy. We’d have to pretend and say everything is fine, when in reality we were dealing with a devastating situation.
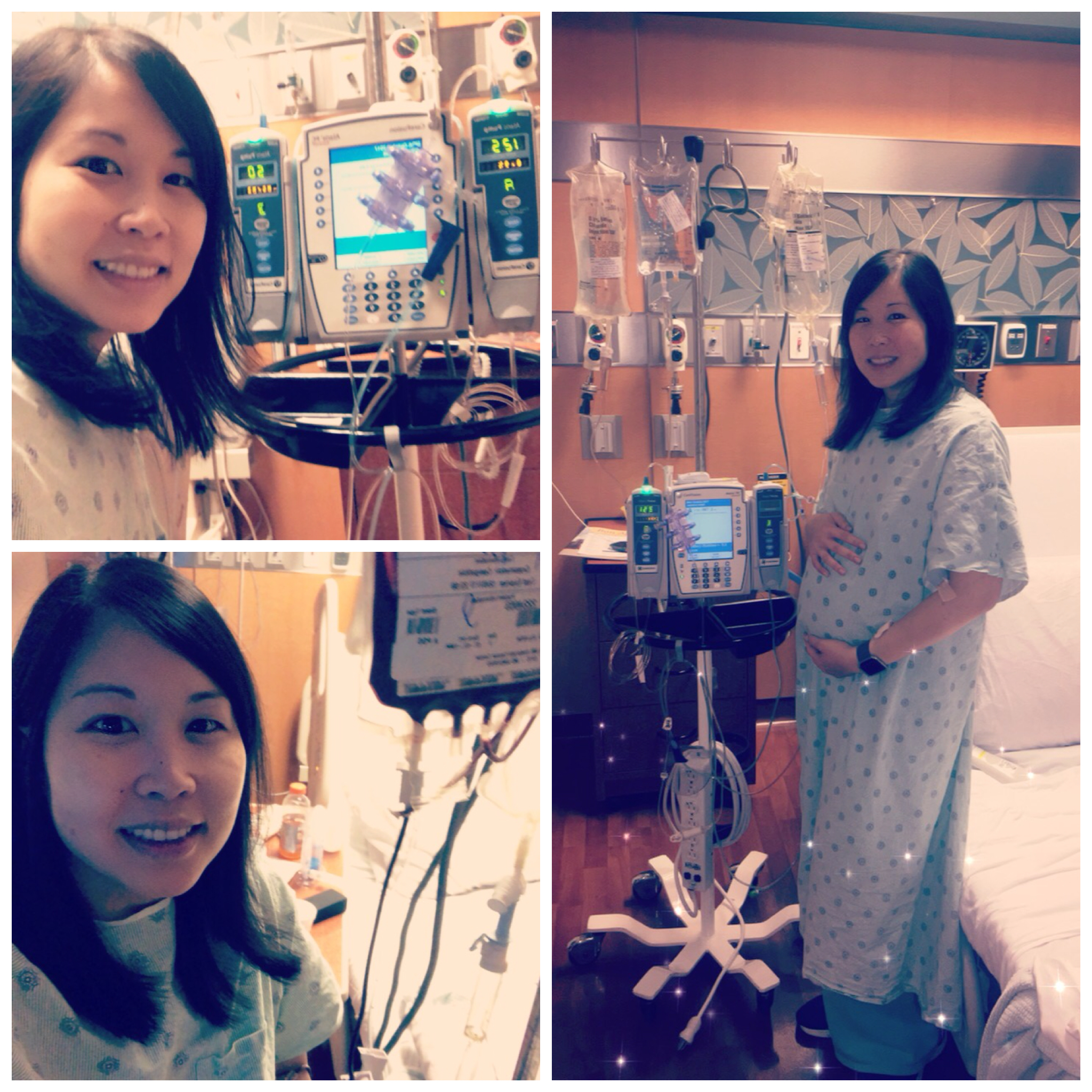
Here we are at Julie’s wedding trying to have fun despite a lot on our mind. I was also in a lot of physical pain since my cancer symptoms were so bad at this point, but I had no idea it was cancer.

We got a call from our genetic counselor two days after the amniocentesis, the Thursday before Julie’s wedding. She shared that our FISH results were in and they were normal! This confirmed that the baby does not have Down Syndrome nor any issues with chromosomes 13, 18 and the sex chromosomes. This was amazing news! Our prayers were being answered. We were on the right path to the NIPT being a false positive. This calmed our nerves and we now felt like we could begin to feel more excited about the pregnancy.
A few days later, Roberto and I were both home from work because we were both sick, including Camila. We got another call from our genetic counselor and our chromosome microarray (second test) results were in. They were normal! This meant that there were no chromosome micro additions or deletions, including mosaicism. It meant that we had more assurance that the other chromosomes didn’t have issues. We continued to move in the direction of getting the false positive we prayed for.
We had one last final test result to wait for–the karyotype. This test result takes the longest to get back, but would give us the final reassurance if the baby had any major genetic issues. We finally got the call two weeks after the amniocentesis. The results were normal! All three of our tests came back with normal results and the healthy baby we prayed for was closer to a reality.
At the time, the genetic counselor and obstetrician can’t explain why I got the NIPT results I did. They want to continue to monitor my pregnancy closely and we’d continue to pray for a healthy baby.
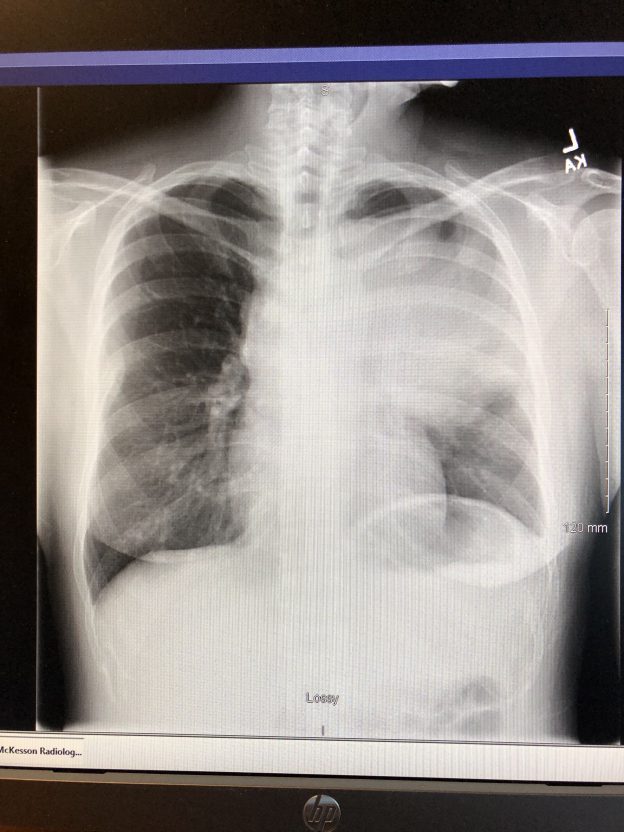
The Link to Cancer
It wasn’t until my cancer diagnosis that my high risk obstetrician stated that the NIPT scare was likely due to me having cancer. She said that cancers that affect the blood, like leukemia and lymphoma, often make it hard for NIPT tests to be properly read. We’re sharing our experience because there’s not much out there on false positive NIPT results, much less how cancer can be linked to it.
I have since shared my diagnoses with our genetic counselor and she’s working with a third party laboratory so I can participate in additional research with them. Hopefully, more will be known and advancements in genetic testing and cancer can be made.
We continue to pray for a healthy baby for the remainder of my pregnancy and chemo treatments. So far, he is doing great and growing well.